Two infectious disease specialists describe and discuss what the scientific community knows about the avian flu virus H5N1 and how pandemic influenza might emerge.
Michael Osterholm, Director, Center for Infectious Disease Research and Policy and Member of the National Science Advisory Board on Biosecurity
Understanding influenza: From the virus to the pandemic.
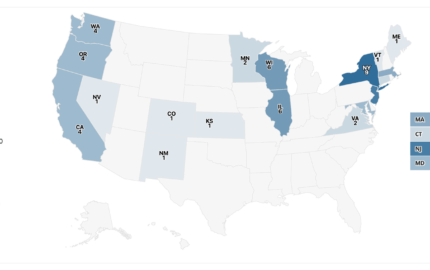
It's not enough for Americans to be worried about influenza in the United States. It's critical that Americans worry about influenza in every country, because we're so dependent on the rest of the world. All that crosses our borders each day in the global just-in-time economy is growing exponentially. And today one out of every nine people who's ever lived is on the face of the earth. If similar to previous pandemics, the numbers will obviously be very large, relative to that world population.
Influenza A viruses are extremely diverse and evolve rapidly. [But] I know less about influenza today than I did 10 years ago, and the more information we get, in many instances, the more questions we have. Influenza pandemics emerge sporadically with variable characteristics. There is no such thing as the influenza pandemic; pandemics differ and are varied, but with one commonality: They're caused by the influenza virus. Influenza causes disease in domestic animals like poultry, horses and swine, and new strains continually emerge. The host range is extensive in birds and mammals. The last count I saw there were 121 different species of birds or mammals that have been infected with H5N1, so just that one strain can be very extensive.
Dealing with other infectious diseases, whether it's mumps, measles, rubella, so many other agents, they are basically glaciers in genetic change compared to the influenza A virus, which is a hurricane in its truest sense. And one of the problems we have today when we talk about H5N1 is there isn't such a thing as an H5N1 virus. There are multitudes of H5N1 viruses, and they're doing different things. They're causing different problems in different areas. Some may actually be more likely to be the next pandemic strain if, in fact, it's going to be at all. There may be specificities for animals vs. humans. Their interrelationship with humans and genetic aspects of humans is all there. This is the part I must tell you I understand less about, and I think many of my colleagues understand less about today, than we did a few years ago. And we're learning a lot, but each week it's almost a new learning experience.
Now to understand pandemic influenza, it occurs when a novel influence of strain emerges from the avian population that has the following features. One, it can be readily transmitted between humans. It's about the birds now, but it's not about the birds once it becomes a human-to-human transmitted agent. That's when we worry about us transmitting to and by ourselves. It will be genetically unique, and clearly we lack immunity to this. Studies have demonstrated over and over again a lack of H5N1 infection in recent history in humans. It is critical for us to understand that we look at influenza through a microscope when we need a telescope. We only have 70-some years of virologic data to really be able to talk about influenza when we know influenza goes back to antiquity.
Today we have this incredible genetic roulette table out there, with billions and billions of poultry to feed the billions and billions of people that we didn't have before. There are more domestic poultry today than we probably have had collectively in the past 1,000 years and so therefore we have this new reservoir. Maybe in a past life this virus would not have been effective enough to basically develop genetic changes, given a limited population. Today it has this unlimited roulette table to play and play and play again, and that is what we're concerned about.
Pandemic influenza is different from avian influenza. If we learn nothing at this meeting, then understand we're not talking about avian influenza as the problem. We're talking about it as the intermediate problem. The problem is pandemic influenza. Now that doesn't mean avian influenza isn't critical, but please distinguish between the two because we keep hearing bird flu, bird flu, bird flu without understanding what we're really talking about is human pandemic influenza as the ultimate outcome of what we're concerned about. [And] influenza pandemics are recurring events. We know that. The world may be on the brink of another pandemic, which was said in very honest and very stark language by the World Health Organization (WHO). All countries will be affected. Widespread illness will occur. Medical supplies will be inadequate. A large number of deaths will occur. Economic and social disruption will be great. RELATED WEB LINK
Ten things you need to know about pandemic influenza.
– who.intEvery country must be prepared, and WHO will alert the world if the pandemic threat increases. [See related link for the October 14, 2005 WHO document: "Ten things you need to know about pandemic influenza."]
Waves of the pandemic: In the 1889-1891 pandemic, it was the third wave, some 12 months into the pandemic that was by far the most severe. In 1918, it was the second wave, some five months into the pandemic that was the most severe. In 1957 and 1968, it was the first wave. From a public policy standpoint, if you have a limited stockpile of anything, which wave do you blow your wad on? Because there won't be the ability to restock in a way that we'd normally think, "OK, we'll get ready for the next season or the next season." That's a critical public policy issue that really hasn't been discussed. The global just-in-time economy presents a unique state of vulnerability to a pandemic. Governments everywhere will have limited resources to respond for 12 to 18 months. Every village, every town, every city, every county, every state, every region, every country will be in the soup about the same time. Resources won't be moving in large numbers, particularly if people want to protect what resources they have for their turn, if the pandemic happens to be slightly off by a couple of weeks in their area. We're going to be on our own. And that's huge. I personally believe that in many instances the developing world is going to do a lot better during pandemic flu than the developed world because they're already used to dealing with subsistence living. They already are hand to mouth. It's going to be the haves that don't realize that when we don't have all these things, things will start to crash.
Hope and despair are not strategies. Yet it's easy to go either way—to hope it's not going to happen and just deny it. And despair, yes. It's clear when you hear this message you could just throw up your hands and say there's nothing I can do about it. What we have to find is that point in between, and the message is there: We'll get through it. Like every pandemic in our history, we'll get through it. The question is how we get through it.
I'd urge all of you to read John Barry's book, "The Great Influenza: The Story of the Deadliest Pandemic in History," in which he has done an amazing job of detailing what 1918-19 was like and why we might have some real important lessons to learn from it. H5N1 has many similarities to the 1918 pandemic's H1N1 virus if you look at the genetic studies and at how it kills in animal models. Today there is evidence that this clinical response may have some very similar pathways, but genetically you look at what it does, and it is very different. Does this mean it's going to happen? No. But it has this ongoing genetic roulette table from which to achieve human-to-human transmission capability with billions of birds out there every day.
In terms of when will it happen? This is an important bottom-line message: No one can predict if, when or where H5N1 virus will shift from an avian strain with incidental human infections to a genetically competent human-to-human RELATED WEB LINK
Unprepared for a Pandemic
– foreignaffairs.orgtransmitted agent. It might never do it. We don't know. But it surely could do it. And there are obviously many warning signs that it may do it, and Asia is going to remain a genetic roulette wheel for H5N1 mutations. I wouldn't want to bet my family's life on H5N1 not becoming the next pandemic influenza strain. That's the only way I know how to express it. So if you want a scientific answer for what's going to happen, I can't give it to you. This is the only answer I can give you.
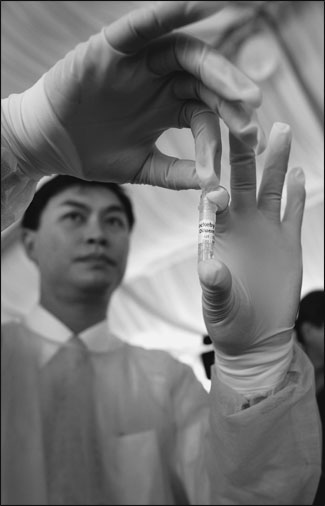
In terms of looking at what might happen, if we look at the next pandemic, most estimate that 30 to 60 percent of the world's population will become infected—60 percent is the very high end based on previous pandemics, and 30 percent is kind of what people see as a low end. If it's a 1968-like pandemic, then there will be two to seven million deaths. If it's a 1918-like pandemic, then there would be 180 to 360 million deaths. In comparison, HIV/AIDS has killed about 25 million people in the past quarter century. When it comes to hospitalization, this kind of a pandemic will obviously swamp the health care system. I believe there is no health care facility in this country that will do an adequate job, or even a beginning job, caring for those who are affected by this pandemic influenza strain. [See related link for Osterholm's article in Foreign Affairs.] One of the major untold stories is what's going to happen to our pharmaceutical drug supply. How many people are going to die from diabetes? If, in fact, we have an international interruption, will the insulin be coming in? Will such people get the drugs they need?
It's very fair to say that there will be certain tipping points in any pandemic, even if it's a moderate pandemic. As we learned in Katrina and in the tsunami, if the dead are treated disrespectfully, without a timely and respectful response, the population's anger increases and its belief in the system goes down. That's going to be a critical piece. We have a just-in-time delivery system for caskets today and for crematorium space. How are we going to plan at our local levels? That won't be a federal issue, won't even necessarily be a state issue. It's going to be a local issue. And the food system today is a just-in-time delivery system. We have very little understanding of that. Literally within days we will see major interruptions of food if we have interruption in travel. With issues of quarantine and border crossings, we need to get statements out now that they're inappropriate responses. They're not going to help. And in fact the collateral damage from doing those things, of interrupting trade and travel, might be a major part of the pandemic we never even thought about or intended. That's important to get that out now: They're not going to work.
To do nothing is unacceptable. To promise protection is unethical. This is the issue we're going to have, and it's going to be our credibility in getting that message out. Governments are going to have limited resources to respond. Count on that now. That's not a failure of government. That's just what the reality will be. Up to 20 to 30 percent of workers will be out at any time due to illness or other ill family members. We see that now with crises that happen, but under the worst-case scenario we're going to survive. Pandemic response will be largely local, so we need to put much more emphasis on local considerations and concerns. Family preparedness is a key issue. The messages have been very fragmented. What can families do if they have the resources? What can families do who don't have the resources now? I can't overemphasize the importance of community leadership, whether it is political, health care, public health, security, first response, business, or even religious. Now is the time to understand the leadership qualities we'll need, like a Winston Churchill or Franklin Delano Roosevelt who says we're in this for the long haul. It's going to get worse before it gets better, but hang with us, we're going to get through it.
In conclusion, as a scientist it's not a matter of if, just when and where. It's just that simple. What we don't know is what it will be like. At minimum, assume we'll have no vaccine for the first six months and then supplies will be trim and limited for the duration. Even if a 1918 scenario does unfold, 98 out of every 100 of us are going to get through this at the other end. The point is how do we get society through it with all of the collateral damage issues. How do we minimize the pain and suffering? What are the messages? Community planning is not an option; it must happen, and we need more emphasis on community planning today.
Marc Lipsitch, Professor of Epidemiology, Harvard School of Public Health
Questions to ask when covering the next infectious disease crisis.
It's possible to report on the kind of topics that we're talking about here, at a very high degree of sophistication, without being a graduate-trained scientist. There's tremendous uncertainty about a lot of the topics here, and there's therefore a lot of disagreement among scientists, mainly on the topics about which we're uncertain. So there's a reason to have multiple sources, good and really knowledgeable sources, to make some sense of where consensus lies. Have curiosity and skepticism, of course, and a desire to fit pieces of information that are coming out at a rapid clip—some 20 to 30 reports each day—into a coherent story. You can't do everything, so the question is which pieces of apparent news (or possible news) fit into a bigger picture and how. One thing that distinguishes a good scientist is a person who doesn't write paper after paper on unrelated observations but understands why and how these observations are relevant to a larger picture. In my small experience with journalism, that offers a pretty good description of the best journalists as well.
There is a lot of information coming out, and the last thing you want to do is contribute to confusion, panic or complacency. One of those three is hard to avoid in any given case; in good news, bad news or mixed news, there can be confusion, complacency and panic. The other aspect is prioritization. With so much news and information and limited space to talk about flu, it's more important to talk perhaps about the mortuary directors once in a while than to w
rite about each press release. Prioritizing news stories will help to make space for the important ones.
What I want to focus more on now is the notion that information very appropriately is managed and for several different reasons—for scientific completeness, for reasons of scientific caution, and for reasons of political or economic caution. When we learn something about a new disease, especially something as publicly important as H5N1, there are at least three different very distinct uses of that information. And the tone with which the information is conveyed might reflect these varying uses. The information is important for scientists to advance the science; it's important for public health workers, who also base their work on the science, to make a response, and this may often be done well before the scientific certainty that scientists like is possible. Finally, there is the work of public health communication. I want to be clear here that the facts and the scientific basis for each of these is the same, and the uncertainty is the same. But scientists have the luxury and also the duty of reserving judgment and not making strong statements until they know, or think they know, what's going on. Communicators and responders have to act whether or not they can be certain. They use the same data, but they use it in a different way.
Public health responders, if they waited until it was certain human-to-human transmission, would have missed their opportunity. So as early responders, particularly for the WHO, which is trying to contain the early spread, there has to be a different standard of evidence, a sort of guilty until proven innocent standard. Action has to be taken before the evidence is in to convict human-to-human transmission. The reasons are obvious: There are delays in getting samples to labs and delays in getting results. And waiting until those delays pass loses time. Beyond that, once the tests are done, there is still some uncertainty.
So the consequence is that if first responders want to have some hope of containing human-to-human transmission, they will have to respond to false alarms. They will have to respond to cases where there is limited or no human-to-human transmission. Unfortunately, perhaps, this same group of people that is supposed to be responding intentionally to false alarms also has the duty of trying to maintain public understanding and public calm.
Human-to-human transmission obviously would trigger changes in the pandemic phase, and the start of pandemic response plans can trigger all sorts of damage, economic and otherwise. Moreover, WHO, less than in the past, is still restricted in its ability to report health information from a country, sometimes formally restricted, and also dependent on the goodwill and cooperation of ministries of health and host governments. So announcements to the public must be cautious and must emphasize the possibility that things are better than they seem, given at the same time that actions must reflect the possibility that they're worse than they seem. Understanding those dynamics helps us to interpret some of the actions and statements.
One question we need to ask is, "What is news in this kind of coverage?" In reporting on press releases from drug companies and health authorities, the real question to ask is how the latest finding changes our understanding about an outbreak or about the situation in a given country or the global situation. Are the claims emphasizing the best or the worst case? How uncertain are we? Or, in other words, how strongly does the evidence support our best guess, because to a greater or lesser degree, all science in an outbreak is framed in uncertainty.
The time frame is enormously important. With almost every response measure, such as a drug or a vaccine or a mask, it is going to be in limited supply. How much will be available when the pandemic starts? How fast, if at all, can production be scaled up? Is planning for the scale-up taking into account the fact that the pandemic itself will be disruptive? Or is that based on current levels of production? With most response measures, you need to understand whether the measure depends on knowing who's infectious and whether that's practical for a given infection. In SARS, it turned out to be practical, but no one knew at the time, how much transmission was happening from asymptomatic or presymptomatic people. So fortunately the answer was yes, it was practical. But we didn't know for sure about that at the time. How strongly can we extrapolate? When we're planning, we have to extrapolate our knowledge of how a particular measure, such as an antiviral drug, worked in the past. What is the basis on which we can expect it to work equally well or better or worse in the next case? In terms of prioritization, and this has not been widely discussed and it's certainly not been carefully planned out, who's going to get the limited supplies? Is there a scientific basis? And is there an ethical basis for this decision?
What mathematical models to date have done is to model how transmission of the virus might be blocked, examining how changes in contact patterns or changes in the course of the infection—if antivirals could make such changes—would alter the epidemic. These models try to reduce the uncertainty in this area. A reporter should be able to get someone to explain the results on the back of an envelope or in a 20-minute phone conversation once they've done their big computer simulation. And there are people who had to make serious decisions based on quantitative predictions. Their view is that underneath it all it might be complicated, but the phenomena are not counterintuitive. Everything modeled is something in our experience, and the models are simply a way of quantifying it and putting it together.