I never realized how seductive a molecule could be. But as I listened to the director of the Medical College of Ohio Cancer Institute speak about this mosaic of proteins, I was surely falling into its spell. It was beguiling, this tiny bit of antibody. In laboratory tests and in rodent studies, it appeared effective against a wide variety of cancers. Sure, the cure rate for mice with cancer is in the miraculous zone when you compare mouse results to results in humans. I knew that. But this antibody—well, maybe it was different.
It seemed to avoid some of the significant pitfalls of other cancer-fighting antibodies. For one thing, it was fully human, with no bits of mouse protein woven into its structure to excite a patient’s immune response. Researchers derived it, in fact, from the antibodies of people with cancer. Also significant was its structure. If you think of the antibody’s well-known Y shape, you’ll recall that it’s the two arms of the Y that vary from one antibody to the next. The rest of the antibody remains the same, no matter what the target. This experimental antibody streamlines the situation, discarding everything but one arm—the variable segment of the antibody that grabs the target cell.
Making a Molecule Into a Story
Perhaps it was my fascination with the science of this antibody that prevented me from thinking clearly about the emotional cost of what I was proposing to my editors at The (Toledo) Blade. The antibody, referred to as H11 by its Canadian manufacturer, Viventia Biotech Inc., was in Phase I clinical trials at the Medical College of Ohio. My proposal: Follow the patients in this trial and see what happens. Let’s use their stories to tell the story of cancer. What it is, how it grows, how we fight it, and how it so often wins.
Two years later, I’m amazed at my naiveté. Think of what I was setting myself up for—not just me, but photographer Jetta Fraser, as well. I knew the basics of the trial: The 12 enrollees were to be people with end-stage disease, people for whom traditional cancer therapies were failing. Although the trial was open to patients with all types of cancers, as long as they lacked central nervous system metastases and maintained reasonably good liver and kidney function, its target were those with no real hope. The bottom line: They should be able to survive three months beyond their treatment.
This was—as is the case with all Phase I trials—not an experiment to see if the new drug worked but an effort to look for adverse reactions and determine a safe dose. In fact, this scrap of antibody would carry no killing agent with it. Although preliminary tests in humans demonstrated H11 targeted tumor cells—and plans were to use it eventually in conjunction with chemotherapy—this step in the process of vetting a promising compound included no lethal accompaniment. There was no reason to think H11 would help patients at all.
I’d essentially planned to do a story about dying people with no real hope of a cure acting as guinea pigs. Intellectually, I think I understood that. Emotionally, I was utterly blind. Seven of the 12 trial participants agreed to let us track their progress. The structure of the final stories dictated including only five of them in the narrative. It focused tightly on two, Cissi Jackson, battling breast cancer since 1992, and Pat Krzeminski, diagnosed with advanced ovarian cancer five years earlier.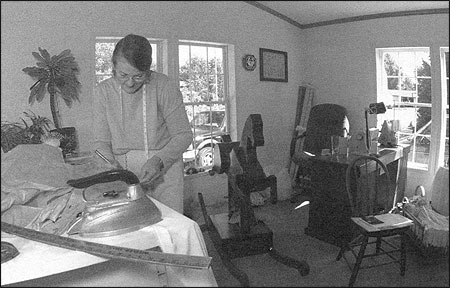
Cissi Jackson worked to finish a wedding dress. During her illness, she continued to create custom-made apparel and upholstery.
Jackson and her daughter Heather at the Infusion Center at the Medical College of Ohio during one of her treatments for breast cancer. Photos by Jetta Fraser/The (Toledo) Blade.
Cancer as a Central Character
From the start, I wanted to make cancer a main character in this series. So my reporting proceeded on two tracks. On one hand, I was interviewing researchers and reading cancer texts and journal articles. This was a challenging world where intricate signals changed the course of a life. I sensed some researchers trying to keep it simple for me, hesitant—no matter how I pushed—to go into the details of their work. Others spent literally hours talking about a world where cells passed messages, evolution’s signature was obvious, and a change in a single protein triggered devastating molecular dominoes.
This world became my emotional haven from the demands of the other reporting track, which required full immersion in the lives of the patients. Jetta and I spent as much time as possible with each patient. We met their families. Some invited us to their doctor’s appointments. Pat Krzeminski in particular welcomed us everywhere. The first time I asked if she’d like us to leave the room when she got into a gown for examination, she laughed. And, no, we shouldn’t leave during her pelvic exam, either.
I don’t think either Jetta or I were prepared for how quickly we snapped into orbit around these women. Each of them entered the trial with impossible hopes. Each could tell me that they signed a consent form that said this was not a test for drug efficacy. And each was certain that this could be their lucky chance.
Pat gave the series its name one day as we followed her in for a doctor’s appointment. She’d just had the back of her head shaved so that it read, “Dr. Fanning No. 1”—James Fanning was her gynecological-oncologist—and if that didn’t draw looks, her cackle did. She stopped to chat with a new patient.
“Don’t you worry about it,” Pat told the newbie as she walked off. “’Cause I’m working on a cure.” Our five-day series was called, “Working on a Cure: Cancer on Trial.” Against all logic, that’s how these patients saw it.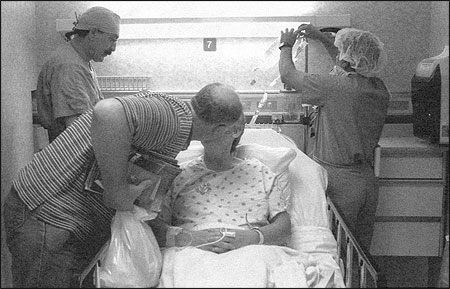
Pat Krzeminski’s husband, Ed, kisses her goodbye before she heads into surgery for her ovarian cancer.
After shaving her head to have it read “Dr. Fanning No. 1,” Krzeminski smiles. Photos by Jetta Fraser/The (Toledo) Blade.
Pat Krzeminski sits with the protocol coordinator after receiving her daily dossage of H11, an experimental cancer treatment.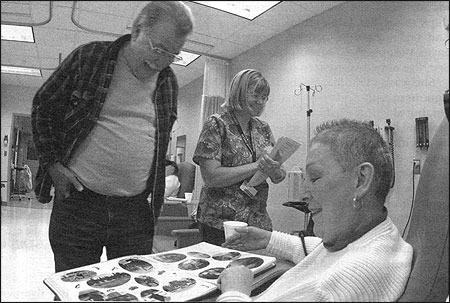
Krzeminski looks at the Memory Book of fellow patient Cissi Jackson as Cissi’s husband, Dave, looks on. Photos by Jetta Fraser/The (Toledo) Blade.
Krzeminski and her daughter Keri in the kitchen of their St. Petersburg, Michigan home.
Krzeminski has an EKG done at the cancer center. Photos by Jetta Fraser/The (Toledo) Blade.
Emotional Entanglements of Coverage
Of course, I knew better. During this trial, had you asked me about Pat’s chances, or the chances of any of these patients, I could have told you the grim truth, as I told editors and co-workers as the story progressed. But those were just words. As I grew more entangled with these women, I was swept in the tsunami of hope that carried them.
Then Cissi Jackson started getting better.
I remember whispering to Jetta early in the reporting that we’d lose Cissi first. She weighed a little over 100 pounds and looked as though one careless jostle would crack her like a dry stick. She was easily the sickest in the initial group of patients we met. Her breast cancer had raged for years. It was in her bones, wrapping her chest and pushing the breath from her lungs.
I confess it drove me a little crazy to listen to her sometimes. In the face of enormous evidence of devastating illness, she exhibited certain hope. She believed lots of things I consider superstitious. Once, she told me, she knew angels sat with her at her sewing table while she worked. And I was puzzled—and privately judgmental—about how little she knew or understood about her disease or its treatment. So when she started to claim she was getting better, I didn’t believe her. I wasn’t the only one.
But she was getting better. Visible lumps of tumor on her head and back vanished. The chest-squeezing shield of tumor disappeared and she stopped using oxygen at night. She gained weight, and the color came back to her face. At one point, her oncologist could find no more sign of cancer.
This went against every predictable outcome for this trial. In the months that followed, her oncologist seemed as puzzled by this turn of events as we were. The oncologist changed her mind more than once about whether it was the H11 behind this turnaround, or another drug Cissi was taking.
No one else had that kind of response to H11. Because of it, Cissi received 100 doses of the antibody, five times more than the trial called for. Her doctor took her off H11 after 10 months and, although Cissi and her husband, Dave, fought to get her back on it, by the time she won that battle, it was too late. Cissi’s liver function crashed. When Jetta and I visited her in late summer—during her effort to go back on the antibody—she was anxious to show us how healthy she was, even jumping on her mini trampoline for our benefit. Maybe she didn’t think we’d notice how winded this demonstration made her, or that we’d miss the huge lump her liver made beneath her shirt.
By this time, I knew a heck of a lot about cancer. I’d interviewed experts all over the country, so I could tell its tale. I also knew that all my college-freshman-psychology-class-certainty about how patients should face disease was utter bullshit. I watched people in the grips of what many folks called denial, and I saw how denial worked for them. These weren’t stupid people. Cissi decided to know what she needed to know about her disease, and that served her incredibly well. Did it keep her alive longer? Who knows? But it kept her happy and, remarkably, heroically peaceful until her death two years after the trial began.
Pat, too, used denial to good ends. Jetta and I were with Pat a lot in the last few weeks of her life. Whenever I visited, if there wasn’t a crowd of others around, she wanted me to interview her. She was relentless. “Ask me another question, Jenni. Ask me another question. Ask me anything. I don’t care. Anything,” she’d say. And I did. But I’d held back on one question until now. It was the thing I was having the hardest time accepting. Pat and I were almost the same age. (I was 48.) I’m making plans, millions of plans, for the future. How did Pat feel about it all ending so soon, so early, too early?
“Does it ever make you mad, that at your age, when you should still have so much time, that it’s all coming to a close now?”
She sucked in her breath. “Oh, that was one thing I don’t want to think about.” She hesitated and teared up a bit, fanning her hands in front of her. “But I said ask anything. So okay, here’s my answer,” she said. “I just don’t think about that. I don’t think about it. And I’m not going to think about it again. I’m going to forget the question. See, I’ve already forgotten it.”
She wasn’t kidding. Maybe the continuous morphine drip helped her forget, but she’d offered me a glimpse at how she managed the last seven years, by not focusing on what she couldn’t change.
A few days later, she was still begging me to ask her questions, but she couldn’t stay awake for her own answers. She’d fall asleep mid-sentence, then suddenly wake up and say something entirely unrelated. “Do you want white meat?” she asked me once. Then she’d realize what she said and laugh until she passed out again. Once she woke up singing the “Cracker Jack” song. Again, she laughed herself to sleep. Those were almost her last words to me, “buy me some peanuts and Cracker Jacks.” She died two days later, death number nine among the 12 who took part in the trial. Three patients are still alive and active, two years after their experimental therapy.
Supposedly, the molecule that seduced us all, H11, is going into Phase II trials for breast cancer. But I’ve been told this for more than a year now, so I’m not certain it will actually happen. I started out so seduced by this molecule. I ended up seduced by hope, by human effort and human frailty. As I wrote in the last installment of the series, after I’d explained to readers how cancer mutations offer cells a sort of eternal life: “If humans had the persistence of cancer, we’d chisel statues to them. Such creative determination is the stuff of heroes. Few of us measure up to the indomitable development of cells run amok. The cruel irony is, cancer requires people of such resolution.”
Jenni Laidman is a science writer at The (Toledo) Blade.