In Bacon County, Georgia, black families are being destroyed by an epidemic of heart disease and diabetes— diseases that are usually caught and treated in white residents. In Essex County, New Jersey, thousands of HIVinfected drug addicts live on the streets of Newark. They don’t vote, don’t have high-powered lobbyists, and are largely ignored by state lawmakers who hand out money for AIDS treatment and drug rehabilitation. And in Mahoning County, Ohio, African-American women are being murdered by husbands, boyfriends and drug dealers so often that public officials appear to have grown used to it.
These counties form the fault line of the nation’s great racial health divide. Although others have documented the nation’s widening racial health gap, many of the places that have been hardest hit hadn’t received much attention. At The Plain Dealer, we spent a year trying to find these places, then we wrote about them in a five-part series published in March 2000.
The Racial Health Gap
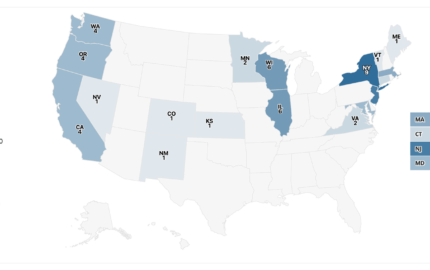
Using the tools of computer-assisted reporting and mortality data gathered from the Centers for Disease Control and Prevention (CDC), we found that a racial health gap exists in virtually every county in the nation with a sizeable number of minority residents. But in what places was the disparity the worst? And why? What characteristics did these fault-line counties have in common?
Ultimately, we concluded that poverty and a lack of health insurance had a profound impact on the widening disparity. But even after these factors were taken into account, we found that African Americans admitted to hospitals receive less medical care than whites who are the same age, same gender, and about as sick. Our analysis of 44.9 million patient stays from 1996 to 1998 found that, compared with the treatment of white patients, doctors were slightly more likely to either just order tests for blacks or administer no treatment at all.
But the idea behind our series was to publish a geography-based analysis of the nation’s racial health disparity, the first-ever county-by-county look at the problem. We believed that by visiting these places and writing about what we found, we might shed light on some larger truth about these hidden tragedies. We believed that by telling the stories of people who were struggling to survive but had never looked into the eye of a reporter or public official, we might contribute new voices to the national discourse and help shape the public health system’s response to these problems.
I don’t know that our stories had any lasting effect. Immediately after they appeared, then-Surgeon General David Satcher praised the stories as a road map for the U.S. Department of Health and Human Services, which had assumed responsibility for developing a national approach. The Ohio Commission on Minority Health distributed 3,000 copies of our stories to its constituents, and my colleague, Elizabeth Marchak, participated in a weekend retreat with 80 black mothers and daughters to explore ways to end violence against women.
Those women were from the Youngstown, Ohio area, which had the nation’s highest murder rate of black women. Still, Youngstown Mayor George McKelvey said our reporting was simply designed to make his city look bad. “I had fun trashing your story on the radio talk shows,” he told us the day after the third installment, when the stories on Youngstown were published. Several days later, 70 black Youngstown residents jammed the city council chambers to protest what they said was the city’s indifference to these killings. The mayor formed a task force to study the problem.
But today, three years later, the task force has been abandoned. Nobody even recalls when it stopped meeting. David Satcher is no longer Surgeon General. And the whole issue of the racial health disparity, which just a short time ago seemed on the brink of becoming a national priority, has been all but forgotten in Washington as our leaders turn their attention to military and security matters.
All that’s left are the stories, stories worth retelling and remembering.
Stories The Plain Dealer Told
They are the stories of people like John Holley, a 47-year-old Lima, Ohio resident who suffered a near-fatal heart attack just days after a doctor refused to see him for chest pain. His wife, Mary, felt certain that the couple’s lack of health insurance was the reason. “When we got there, the doctor said, ‘I don’t understand why they sent you here. I’m not going to touch you,’” his wife recalled. “I was so shocked. I just said, ‘Thank you.’”
They are the stories of people like Maxine and Cynthia Wright of Youngstown, who share a bond beyond most mothers and daughters: Each lost a child to homicide. “It is hell,” Maxine said wearily.
And they are the stories of Harold Moore, who was partially paralyzed from a drug overdose and lay dying from AIDS in a hospital bed at the Broadway House, a home for indigent AIDS patients in Newark. Drug-addicted, homeless, forgotten men like Moore wander the streets of Newark and the other northern New Jersey cities that lie in the shadow of Manhattan, whose brightly lit skyscrapers seem to taunt this boarded-up city from across the Hudson River.
Here, women sell themselves for $15. Men run heroin. Using dirty needles, they shoot up behind abandoned buildings, in cemeteries or in public bathrooms. They are spreading HIV, the virus that causes AIDS, at a pace that rivals some Third World nations. They are overwhelmingly black, and we called them “The Lost Ones” because, despite being desperately ill from AIDS, they did not seek medical treatment. They have no addresses. They have no telephones. They have no hope.
In Essex County, where black residents were dying from AIDS at 10 times the rate of whites, poverty and affluence live side-by-side, creating one of the widest racial health gaps we could find in the nation. “When I was out on the street, I had lost all my moral value, my self-respect,” Moore said. “All that flies out the window when you use drugs.”
Moore’s story was sad, compelling and uplifting, all at the same time. On some days, when he felt okay, he went in his wheelchair to speak to groups about “living with the virus.” While he was sick, for the first time in his life he spent time with his mother, becoming the son he had never been as he came to recognize the importance of family and friends. Lying in his hospital bed, through his tears, he told us something amazing, “I wouldn’t change these last seven years for nothing.”
Transforming Data Into Stories
Our deathbed interview with Moore became the foundation upon which we built the fourth day of our five-day series. His words gave us the ability to share his story with our readers, and that was the payoff we received for more than 200 hours that we’d spent querying the CDC’s online mortality database (wonder.cdc.gov).
As we began our reporting, we ran death rates, by race and gender, for the nearly 1,200 counties in the United States. Then, we imported the results into a database. Armed with this powerful data, we started talking with health officials and experts around the country. Few of them knew what we were talking about. Nobody had ever seen numbers like we had tallied. Many local and state public health officials simply told us we were wrong, though they could not offer us different numbers. Others—when confronted with data showing these disparities—denied there was any problem in their county or state. And some refused to talk to us.
Even so, the problems of minority health are not unknown to public health officials, especially those in federal agencies and at universities. In our search for information, we’d found studies and federal grants, involving all sorts of bureaucracies, devoted to—but not necessarily solving—a myriad of minority health problems.
As we traveled the nation and our state, one thing became increasingly clear: People working on the ground (on the streets, in public clinics, and community health centers) understood the scope of the tragedy and were scrambling to solve the problem on their own, often with little or no institutional support.
Two nurses in Lima, a depressed industrial city that sprouted up in the middle of central Ohio’s cornfields, were working in the city’s worst neighborhood, trying to catch untreated high blood pressure and diabetes before the diseases became disabling. In Youngstown, the Ursuline Nuns weren’t waiting for any of the city’s boards or commissions to act on the city’s homicide epidemic. For nearly a decade, they had been buying up old homes and filling them with single moms and their kids. The nuns knew, after 125 years in the city, that preserving families would help rebuild the community. It was their investment in the next generation, they said.
And in Cincinnati, a group of doctors and nurses had given up the comfort of private-practice medicine to start a clinic in an abandoned elementary school in Cincinnati’s over-the-Rhine district, a neighborhood split evenly between poor Appalachian whites and inner-city blacks and Hispanics. Patients were asked to pay what they could based on their income. Doctors at the Crossroads Health Center said they saw more similarities than differences in the white, black and Latino patients they treated.
People Respond to the Reporting
Reaction to the series was swift. The frontline health care workers we had interviewed all applauded the stories. They took them as a sort of call to action, proof of what they had been trying so hard to communicate to others about the problems they were treating. But those above them—high-ranking hospital administrators and public health officials at the state and county level—didn’t respond, even though we sent them copies of the stories and offered to publish their reaction.
We received hundreds of telephone calls, letters and e-mail from readers. Many wanted to tell us their personal stories. Many more simply wanted to express their appreciation. I was surprised, time after time, to hear callers tell me that they were shocked that our newspaper would undertake such a project. “How did I manage to do this story?” they asked.
I understood that many young people felt detached from daily newspapers. I knew that poor people felt this way. But many of the callers were educated professionals. To hear them talk about their distrust of news organizations was eye opening.
Our stories also became a bridge to our African-American readers, people who had buried too many in their family before their time. One elderly woman who met me in person was surprised to discover that I am white. She gave me a bear hug and whispered in my ear, “I didn’t think white people cared.”
Dave Davis is an investigative reporter for The Plain Dealer in Cleveland, Ohio, who has specialized in health care issues.
These counties form the fault line of the nation’s great racial health divide. Although others have documented the nation’s widening racial health gap, many of the places that have been hardest hit hadn’t received much attention. At The Plain Dealer, we spent a year trying to find these places, then we wrote about them in a five-part series published in March 2000.
The Racial Health Gap
Using the tools of computer-assisted reporting and mortality data gathered from the Centers for Disease Control and Prevention (CDC), we found that a racial health gap exists in virtually every county in the nation with a sizeable number of minority residents. But in what places was the disparity the worst? And why? What characteristics did these fault-line counties have in common?
Ultimately, we concluded that poverty and a lack of health insurance had a profound impact on the widening disparity. But even after these factors were taken into account, we found that African Americans admitted to hospitals receive less medical care than whites who are the same age, same gender, and about as sick. Our analysis of 44.9 million patient stays from 1996 to 1998 found that, compared with the treatment of white patients, doctors were slightly more likely to either just order tests for blacks or administer no treatment at all.
But the idea behind our series was to publish a geography-based analysis of the nation’s racial health disparity, the first-ever county-by-county look at the problem. We believed that by visiting these places and writing about what we found, we might shed light on some larger truth about these hidden tragedies. We believed that by telling the stories of people who were struggling to survive but had never looked into the eye of a reporter or public official, we might contribute new voices to the national discourse and help shape the public health system’s response to these problems.
I don’t know that our stories had any lasting effect. Immediately after they appeared, then-Surgeon General David Satcher praised the stories as a road map for the U.S. Department of Health and Human Services, which had assumed responsibility for developing a national approach. The Ohio Commission on Minority Health distributed 3,000 copies of our stories to its constituents, and my colleague, Elizabeth Marchak, participated in a weekend retreat with 80 black mothers and daughters to explore ways to end violence against women.
Those women were from the Youngstown, Ohio area, which had the nation’s highest murder rate of black women. Still, Youngstown Mayor George McKelvey said our reporting was simply designed to make his city look bad. “I had fun trashing your story on the radio talk shows,” he told us the day after the third installment, when the stories on Youngstown were published. Several days later, 70 black Youngstown residents jammed the city council chambers to protest what they said was the city’s indifference to these killings. The mayor formed a task force to study the problem.
But today, three years later, the task force has been abandoned. Nobody even recalls when it stopped meeting. David Satcher is no longer Surgeon General. And the whole issue of the racial health disparity, which just a short time ago seemed on the brink of becoming a national priority, has been all but forgotten in Washington as our leaders turn their attention to military and security matters.
All that’s left are the stories, stories worth retelling and remembering.
Stories The Plain Dealer Told
They are the stories of people like John Holley, a 47-year-old Lima, Ohio resident who suffered a near-fatal heart attack just days after a doctor refused to see him for chest pain. His wife, Mary, felt certain that the couple’s lack of health insurance was the reason. “When we got there, the doctor said, ‘I don’t understand why they sent you here. I’m not going to touch you,’” his wife recalled. “I was so shocked. I just said, ‘Thank you.’”
They are the stories of people like Maxine and Cynthia Wright of Youngstown, who share a bond beyond most mothers and daughters: Each lost a child to homicide. “It is hell,” Maxine said wearily.
And they are the stories of Harold Moore, who was partially paralyzed from a drug overdose and lay dying from AIDS in a hospital bed at the Broadway House, a home for indigent AIDS patients in Newark. Drug-addicted, homeless, forgotten men like Moore wander the streets of Newark and the other northern New Jersey cities that lie in the shadow of Manhattan, whose brightly lit skyscrapers seem to taunt this boarded-up city from across the Hudson River.
Here, women sell themselves for $15. Men run heroin. Using dirty needles, they shoot up behind abandoned buildings, in cemeteries or in public bathrooms. They are spreading HIV, the virus that causes AIDS, at a pace that rivals some Third World nations. They are overwhelmingly black, and we called them “The Lost Ones” because, despite being desperately ill from AIDS, they did not seek medical treatment. They have no addresses. They have no telephones. They have no hope.
In Essex County, where black residents were dying from AIDS at 10 times the rate of whites, poverty and affluence live side-by-side, creating one of the widest racial health gaps we could find in the nation. “When I was out on the street, I had lost all my moral value, my self-respect,” Moore said. “All that flies out the window when you use drugs.”
Moore’s story was sad, compelling and uplifting, all at the same time. On some days, when he felt okay, he went in his wheelchair to speak to groups about “living with the virus.” While he was sick, for the first time in his life he spent time with his mother, becoming the son he had never been as he came to recognize the importance of family and friends. Lying in his hospital bed, through his tears, he told us something amazing, “I wouldn’t change these last seven years for nothing.”
Transforming Data Into Stories
Our deathbed interview with Moore became the foundation upon which we built the fourth day of our five-day series. His words gave us the ability to share his story with our readers, and that was the payoff we received for more than 200 hours that we’d spent querying the CDC’s online mortality database (wonder.cdc.gov).
As we began our reporting, we ran death rates, by race and gender, for the nearly 1,200 counties in the United States. Then, we imported the results into a database. Armed with this powerful data, we started talking with health officials and experts around the country. Few of them knew what we were talking about. Nobody had ever seen numbers like we had tallied. Many local and state public health officials simply told us we were wrong, though they could not offer us different numbers. Others—when confronted with data showing these disparities—denied there was any problem in their county or state. And some refused to talk to us.
Even so, the problems of minority health are not unknown to public health officials, especially those in federal agencies and at universities. In our search for information, we’d found studies and federal grants, involving all sorts of bureaucracies, devoted to—but not necessarily solving—a myriad of minority health problems.
As we traveled the nation and our state, one thing became increasingly clear: People working on the ground (on the streets, in public clinics, and community health centers) understood the scope of the tragedy and were scrambling to solve the problem on their own, often with little or no institutional support.
Two nurses in Lima, a depressed industrial city that sprouted up in the middle of central Ohio’s cornfields, were working in the city’s worst neighborhood, trying to catch untreated high blood pressure and diabetes before the diseases became disabling. In Youngstown, the Ursuline Nuns weren’t waiting for any of the city’s boards or commissions to act on the city’s homicide epidemic. For nearly a decade, they had been buying up old homes and filling them with single moms and their kids. The nuns knew, after 125 years in the city, that preserving families would help rebuild the community. It was their investment in the next generation, they said.
And in Cincinnati, a group of doctors and nurses had given up the comfort of private-practice medicine to start a clinic in an abandoned elementary school in Cincinnati’s over-the-Rhine district, a neighborhood split evenly between poor Appalachian whites and inner-city blacks and Hispanics. Patients were asked to pay what they could based on their income. Doctors at the Crossroads Health Center said they saw more similarities than differences in the white, black and Latino patients they treated.
People Respond to the Reporting
Reaction to the series was swift. The frontline health care workers we had interviewed all applauded the stories. They took them as a sort of call to action, proof of what they had been trying so hard to communicate to others about the problems they were treating. But those above them—high-ranking hospital administrators and public health officials at the state and county level—didn’t respond, even though we sent them copies of the stories and offered to publish their reaction.
We received hundreds of telephone calls, letters and e-mail from readers. Many wanted to tell us their personal stories. Many more simply wanted to express their appreciation. I was surprised, time after time, to hear callers tell me that they were shocked that our newspaper would undertake such a project. “How did I manage to do this story?” they asked.
I understood that many young people felt detached from daily newspapers. I knew that poor people felt this way. But many of the callers were educated professionals. To hear them talk about their distrust of news organizations was eye opening.
Our stories also became a bridge to our African-American readers, people who had buried too many in their family before their time. One elderly woman who met me in person was surprised to discover that I am white. She gave me a bear hug and whispered in my ear, “I didn’t think white people cared.”
Dave Davis is an investigative reporter for The Plain Dealer in Cleveland, Ohio, who has specialized in health care issues.