Coverage of Terrorism
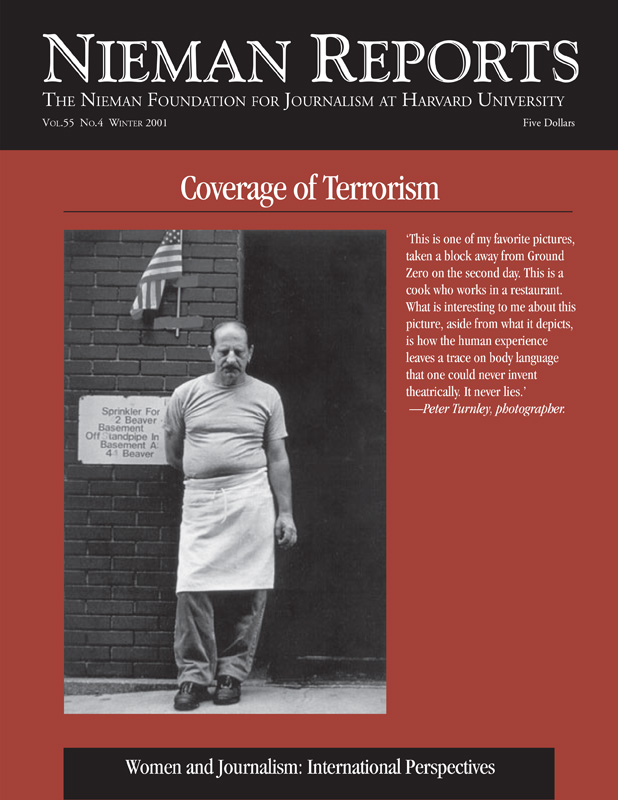
Through the night of September 11, 2001, photographer Peter Turnley took refuge in a second-floor office in a clothing store, its windows blown out by the force of the attack on the World Trade Center. As he tried to absorb what he was seeing, he documented the devastation. At dawn, he moved close to the site and fastened his journalistic eye on faces whose expressions evoke our feelings of loss. From covering war, Turnley knew that “the most important pictures…are after the battle, when one sees the human impact.”
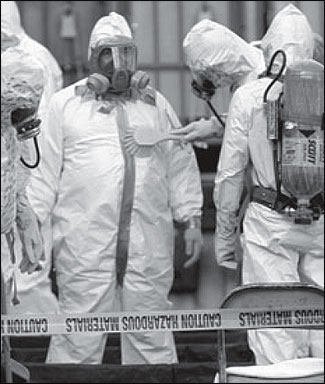
A hazardous-materials response team during a decontamination process. Photo by Tom Mihalek, courtesy of Agence France-Presse.
RELATED ARTICLE
"Highlighting Antibiotic Resistance"During the impressive print and electronic media coverage of recent events concerning the threat of bioterrorism through anthrax dissemination, one major threat has been almost completely ignored by the press. It is that posed by the widespread and indiscriminate use of antibiotics to “treat” perceived but perhaps not real exposure to anthrax spores. This is a major omission and has potentially disastrous consequences.
Humans, together with almost every other biological creature, live side by side with or actually act as hosts to other organisms, including large numbers of bacteria. Under normal conditions, bacteria live on our skin, in our nasal passages, and in our intestines. Examples of such organisms include strains of E. coli (intestines), staphylococcus and streptococcus (skin, respiratory and oral passages), and various fungi (skin and respiratory passages).
All animals, including humans, have developed pretty effective ways of maintaining defenses against uncontrolled proliferation of these bacteria. Occasionally, we are infected by organisms that we encounter routinely in our daily environments—meaning that we have encountered an unusual strain to which we have no immunity or our immune systems are compromised, as in the case of HIV. When normally harmless microorganisms—those a normal immune system can keep in check—gain the upper hand and are able to multiply within our bodies to an abnormal extent, we are said to be infected by them.
During the past 75 years or so, we have developed various chemical and biologic agents that are more toxic to microorganisms than they are to humans and are therefore useful in supplementing our natural defenses against microorganisms. Examples of these include so-called chemotherapeutic agents (such as sulfonamides) and antibiotics, such as penicillin and tetracyclines. Ciprofloxin (Cipro) now considered to be the “treatment of choice” (but not the only treatment) of anthrax is an antibiotic. These agents are extremely valuable in restoring the delicate equilibrium we maintain with other biological creatures with which we (usually) peacefully coexist when they have gained the upper hand for one of the reasons mentioned earlier.
But their use is not without risks. And their indiscriminate and inappropriate use is positively dangerous, yet this very real danger has not adequately been brought to the public’s attention as part of the reporting on anthrax.
Our bodies are normally inhabited by hundreds of millions of individual bacteria of dozens of strains. Like humans, these individual bacteria differ from one another in a variety of ways. One of the differences most important to us is in their degree of sensitivity to antibiotics. Some individual bacteria are rather easily killed by these drugs, and others are more resistant to them. When antibiotics are taken, the most susceptible bacteria are killed first and the least susceptible last. Sometimes the bacteria most resistant to antibiotics are not killed at all, leaving them free to multiply after the course of drugs is discontinued.
When this happen, we have used our own bodies as a medium for breeding an antibiotic-resistant strain of the very bacteria we are trying to control. In doing so, we have created a situation that is worse than if we had not attempted antibiotic treatment at all, since the competition for food and other resources provided by the antibiotic sensitive bacteria that had held the growth of the resistant strains in check has been removed. When the antibiotics are discontinued, the resistant strains of bacteria are able to grow without restraint, and the infection returns—but this time in a pure antibiotic resistant form.
The use of antibiotics without specific indications, in inadequate dosage or for an insufficient period of time, is much worse than not using them at all. The recent emergence of drug-resistant strains of tuberculosis and staphylococcus are examples of the result of inappropriate and indiscriminate antibiotic use—in humans and animals.
If the hysteria—much of it fanned by media coverage regarding real or perceived threats from anthrax or other biological agents—continues without counterbalancing caution against the indiscriminate use of antibiotics and other drugs, it is quite likely that hundreds of thousands or millions of people will have begun inappropriate or ineffective courses of treatment, leading to the widespread development of drug-resistant strains of not only anthrax, but other bacteria as well. This poses a threat not only to those individuals directly involved in such treatment, but also to anyone else to whom the drug-resistant strains can be passed.
This very real possibility is at least as great if not a greater threat to the public health than that of direct attack by anthrax or any other biological agent.
Where is the leadership likely to come from in giving this important message the prominence it deserves? It is unlikely that the pharmaceutical industry—which is after all like other industries a revenue, profit and shareholder value-driven entity—will be at the forefront of cautioning the public against the inappropriate and excessive use of their products. They are currently in the midst of a multimillion (if not billion) dollar campaign of marketing prescription drugs to the general public. Most of these drugs have very proscribed and limited indications. Many of them have less expensive and equally or more effective generic counterparts. Therefore, the track record of the pharmaceutical industry in acting in the broad public interest as opposed to the narrow interests of their shareholders is not comforting.
These ad campaigns put pressure on physicians to prescribe drugs when they might otherwise not do so. But they are likely to be highly effective even without the complicity of physicians due to the increasing availability of antibiotics and other drugs over the Internet without prescriptions.
It is equally unlikely that our political leaders will provide the necessary leadership on this issue. With few exceptions, they lack the expertise to do so. In addition, it seems to go against the popular American response to pop a pill as an answer to almost every problem and may therefore be seen by many as an unpopular position for a politician to take. And this message may not be seen by the pharmaceutical industry, perennially one of the nation’s leading contributors to political campaigns, to be friendly to them.
That leaves the public relying upon journalists, using their traditional role of digging up the facts and publishing them, as the best hope for getting this message out. The trend in recent years has been for ratings to drive coverage as evidenced by how reporting on the incidence of anthrax has far outpaced a story such as this one, even though the level of harm it can alert people to might potentially be much higher.
The anthrax scare has also uncovered serious deficiencies in our system of public health surveillance and services. But these deficiencies were hardly a secret even before anthrax. Just last year Laurie Garrett, a highly respected journalist, published a book called “Betrayal of Trust: The Collapse of Global Public Health,” that received a flurry of attention in the “elite” media at the time but was never picked up in the popular media, particularly television. We seem to have a great deal of trouble paying much attention to serious—but not dramatic—problems, especially if they involve the sacrifice of short-term personal gratification for long-term societal goals. Where is the coverage of the long-term implications of the Bush tax cuts (“the people know better how to spend their money than the government does”) for programs such as our public health infrastructure? There are many more examples.
Increasingly, news coverage has come to be driven by the bottom line more than the news value or public importance of a story. Let’s hope this important story is an exception. Let’s hope journalism is up to the task.
Philip Caper, M.D. is an adjunct lecturer at the Harvard School of Public Health and an internationally recognized expert on patterns of medical practice.


